Migraine, a common neurological issue, often manifests as severe headaches typically on one side of the head, accompanied by nausea, vomiting, and sensitivity to light and sound.
Affecting about 14% of people globally, it’s more prevalent in women and can significantly impact individuals, families, and society.
In this article, we explore the genetics of migraines, examining how hereditary traits might influence their occurrence.
Let’s dive in!
Quick Note:
Looking for a quick answer?
A family history of migraines can increase your likelihood of experiencing them, with a 50-75% higher chance if your relatives suffer from migraines. This link indicates that certain genetic components contribute to migraine susceptibility.
While genetics play a significant role in migraines, suggesting a hereditary aspect, it’s not the only factor.
Environmental factors, such as stress, diet, hormonal changes, and specific medications, also have a crucial role in triggering or aggravating migraines. These external elements interact with individual genetic predispositions, affecting each person’s migraine risk and experience differently.
Therefore, migraines are a complex interplay of genetic and environmental factors. For an in-depth exploration of the genetic basis of migraines, their types, triggers, and effective management strategies, continue reading this article.
Are Migraine Genetic?
Yes, migraines have a significant genetic component. Research suggests that genetics account for about 50-75% of the susceptibility to migraines, indicating a strong hereditary influence.
If you have family members who experience migraines, you’re more likely to suffer from them as well. This genetic predisposition makes individuals more sensitive to environmental triggers that can provoke migraine attacks, such as stress, certain foods, or changes in weather.
So, Are Migraines Hereditary?
Migraines indeed have a hereditary basis, with genetics accounting for 50-75% of the risk, playing a critical role in determining one’s risk of developing migraines.
However, it’s important to note that while genetics lay the foundation for migraine susceptibility, environmental factors, and lifestyle choices also have a significant impact.
Together, these elements interact to influence who gets migraines and how severely they experience them.

Genetic Roots of Migraine
Migraines are generally categorized into two types based on their genetic origins:
Monogenic Migraines
Rare and directly caused by changes in a single gene. An example is familial hemiplegic migraine (FHM), where mutations in specific genes affect brain cell communication.
Some of the key genes involved include:
- CACNA1A: This gene encodes a protein that forms a part of a calcium channel in nerve cells. Mutations in CACNA1A can lead to familial hemiplegic migraine (FHM1), where altered ion flow in neurons affects neurotransmission, triggering migraine symptoms.
- ATP1A2: Associated with FHM2, mutations in this gene disrupt the function of a protein essential for maintaining the balance of sodium and potassium ions in nerve cells. This imbalance can lead to migraine with aura, marked by visual disturbances preceding the headache.
- SCN1A: Linked to FHM3, mutations in SCN1A affect sodium channels in nerve cells, which are critical for the transmission of electrical signals in the brain. These mutations can cause severe migraine symptoms, including hemiplegia (temporary paralysis on one side of the body).

Polygenic Migraines
More common, involving multiple genes each contributing to a small extent. This type includes migraines with and without aura and is influenced by both genetic and environmental factors.
Some of the genes and their roles include:
- TRPM8: This gene is involved in temperature sensation and has been associated with migraines. Variations in TRPM8 may influence the brain’s response to environmental triggers like temperature changes, potentially leading to migraines.
- LRP1: The LRP1 gene plays a role in lipid metabolism and neuronal communication. Genetic variations in LRP1 have been linked to an increased risk of common migraine types, suggesting its role in brain signaling pathways.
- MEF2D: Involved in neuronal development and survival, MEF2D mutations have been associated with migraine susceptibility. These mutations may impact brain cell function and response to environmental factors, contributing to migraine development.
- PHACTR1: This gene is implicated in vascular and neuronal functions. Variations in PHACTR1 have been linked to migraines, particularly influencing blood vessel function in the brain, which can trigger migraine symptoms.
- TGFBR2: Transforming growth factor-beta (TGF-β) signaling, influenced by TGFBR2, plays a role in the development and maintenance of blood vessels. Mutations in TGFBR2 have been associated with an increased risk of migraines, possibly due to altered vascular integrity and response.
While monogenic migraines are directly linked to specific gene mutations, polygenic migraines result from a complex interplay of multiple genes and environmental factors, contributing to the more common forms of migraine experienced by individuals.
Understanding these genetic contributions is crucial for developing targeted treatments and personalized management strategies for migraine sufferers.
Understanding the Genetic Pathways
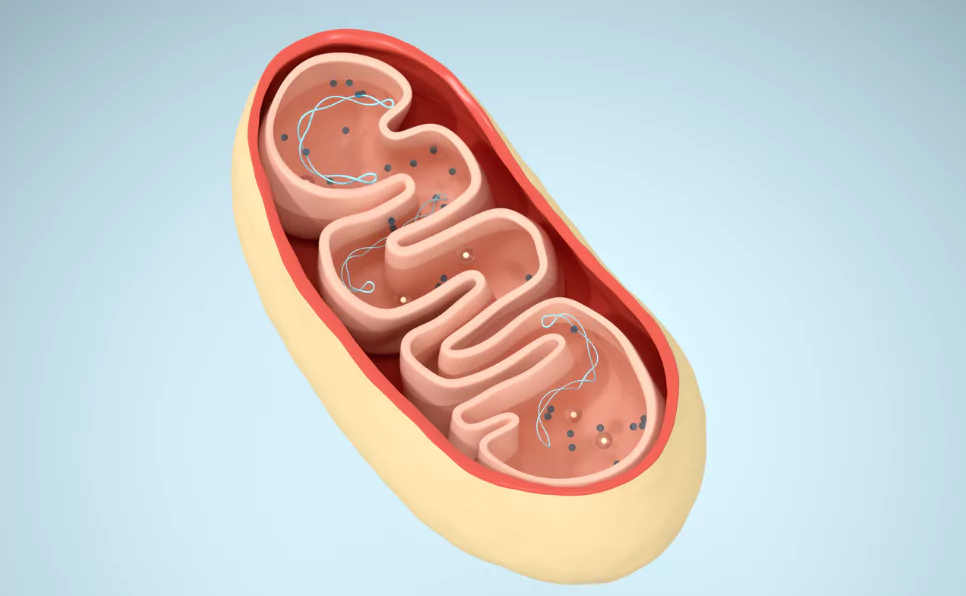
Several key genetic pathways have been implicated in migraines. These include:
- Ion Channel Pathway: Changes in genes regulating ion flow can affect brain cell communication and pain signaling.
- Neurotransmitter Pathway: Variations in genes involved in neurotransmitter production can influence brain function and behavior, often seen in migraine comorbidities like depression.
- Vascular Pathway: Genes controlling vascular function can impact blood flow and inflammation, potentially triggering migraines.
Research Methods & Challenges in Migraine Genetics
- Twin and Family Studies: These studies estimate the genetic contribution to migraines by comparing the occurrence of migraines in twins and among family members.
- Genome-Wide Association Studies (GWAS): These studies scan the entire genome to identify genetic markers associated with migraines.
- Candidate Gene Studies: These focus on specific genes and their roles in migraines, validating and expanding upon GWAS findings.
Genetic research has shed light on migraine pathophysiology, emphasizing the role of the neurovascular unit (neurons, glial cells, and blood vessels) in migraines.
It also points to genetic links between migraines and conditions like depression and hypertension, suggesting shared underlying mechanisms.
However, challenges remain in migraine genetic research, including:
- Identifying the specific genes and variants among many associated with migraines, especially since many are in non-coding regions of the genome.
- Understanding how these genetic factors affect cell and molecular functions, requiring detailed studies.
- Investigating how different genetic factors and environmental influences combine to affect migraine risk and symptoms.
- Applying genetic research to clinical practice, like developing genetic tests for better migraine diagnosis and treatment.
Migraine and Comorbid Conditions
Migraines often co-occur with other health issues like depression, anxiety, and cardiovascular diseases.
Research has shown that these conditions might share common genetic causes with migraines.
For instance, genetic areas linked to migraines are also related to neurological and psychiatric disorders, indicating overlapping biological pathways.
Understanding the shared genetic factors between these conditions is crucial, as it can inform better management and treatment strategies.
The Role of Environment in Migraine Triggers
While genetics are a significant factor, environmental aspects also play a critical role in triggering migraines.
Factors such as stress, diet, hormonal changes, and certain medications can influence the onset and severity of migraines.
These environmental triggers interact with genetic predispositions, affecting individuals differently based on their unique genetic makeup.
The Future of Migraine Treatment: Personalized Medicine
Advancements in understanding migraine genetics have opened the door to personalized medicine, where treatments can be tailored to an individual’s genetic profile.
This approach can lead to more effective and suitable treatment options, considering the type of migraine and individual response.
The Role of Genetics in Migraine Management
Understanding the genetic links is crucial for comprehensive migraine management.
It helps in early diagnosis, informs treatment strategies, and opens the door to personalized medicine, where treatment is tailored based on an individual’s genetic makeup.
Lifestyle and Migraines: The Environmental Connection
Lifestyle factors such as sleep, exercise, diet, stress management, and keeping a migraine diary play a significant role in migraine management.
These factors can either trigger or alleviate migraine symptoms, depending on individual genetic sensitivities.
FAQs
Which Gender Has More Migraines?
Women are more likely to experience migraines than men. Studies indicate that migraines affect approximately 18% of women and 6% of men in the United States. This disparity is largely attributed to hormonal differences, especially fluctuations that women experience during their menstrual cycle, pregnancy, and menopause.
Are Migraines Dominant or Recessive?
The inheritance pattern of migraines is complex and not strictly classified as dominant or recessive. Migraines are considered a multifactorial condition, influenced by multiple genes and environmental factors. This means that the risk of developing migraines is affected by the interaction of several genes, rather than a single dominant or recessive gene.
Does Caffeine Help Migraines?
Caffeine can have both positive and negative effects on migraines. For some, a moderate amount of caffeine may help relieve migraine symptoms by narrowing the blood vessels and blocking certain pain pathways. However, excessive caffeine consumption or withdrawal can trigger migraines in others. It’s important to monitor how caffeine affects your migraines and adjust your intake accordingly.
What Autoimmune Disease Causes Migraines?
While migraines are not directly caused by autoimmune diseases, individuals with certain autoimmune conditions, such as lupus or rheumatoid arthritis, may be more prone to experiencing migraines. The inflammation and immune system activity associated with these conditions can contribute to migraine development and severity.
Are Migraines Hereditary from Mother?
Migraines can be hereditary, and it’s possible to inherit a predisposition to migraines from either parent, not just the mother. However, if a mother suffers from migraines, the likelihood of her children experiencing migraines increases, indicating a genetic link.
Final Words On Genetics of Migraines
Migraines are a complex condition influenced by a mix of genetic and environmental factors.
Further, the genetic landscape of migraines is also intricate and not fully understood.
While current genetic insights partially explain why migraines run in families, much remains to be discovered.
Future research, involving more diverse and larger populations and advanced gene sequencing techniques, is needed to deepen our understanding of migraines.
Understanding these aspects is crucial for developing effective prevention and treatment strategies.
In sum, while migraines can indeed be hereditary, the interplay between genetics and environmental factors is intricate, highlighting the need for a multifaceted approach to understanding and treating this condition.
References:
- Genetics of migraine: where are we now? | The Journal of Headache and Pain
- Advances in genetics of migraine | The Journal of Headache and Pain
- Genetics and migraine – The Migraine Trust
- Comorbidities of Migraine | American Migraine Foundation
- Comorbid and co-occurring conditions in migraine and associated risk of … | The Journal of Headache and Pain
- Are Migraines Hereditary? – Cleveland Clinic
- The Genetics of Migraine | American Migraine Foundation
- Lifestyle Changes for Migraine | American Migraine Foundation
- Lifestyle factors and migraine – The Lancet
- Frontiers | Lifestyle Modifications for Migraine Management
- What Causes Migraine | American Migraine Foundation
- Glia Signaling and Brain Microenvironment in Migraine – Springer

Dr. Sumeet is a seasoned geneticist turned wellness educator and successful financial blogger. GenesWellness.com, leverages his rich academic background and passion for sharing knowledge online to demystify the role of genetics in wellness. His work is globally published and he is quoted on top health platforms like Medical News Today, Healthline, MDLinx, Verywell Mind, NCOA, and more. Using his unique mix of genetics expertise and digital fluency, Dr. Sumeet inspires readers toward healthier, more informed lifestyles.





Herbal remedies are preferred by many who seek a more holistic and natural approach to treating their headaches. They could be a good alternative to over-the-counter or prescription medications.Many herbs and plants, including lavender, peppermint, ginger, and feverfew, are thought to be effective headache remedies. Each person may react differently to any given plant.It is essential to speak with a healthcare provider before using herbal remedies, especially if you have severe or persistent headaches.