Type 2 diabetes happens when the body has trouble using sugar, or glucose, correctly as a source of energy. This can lead to high sugar levels in the blood, causing issues with the heart, nerves, eyes, kidneys and other parts of the body.
Type 2 diabetes is a serious health problem that affects many people worldwide. As stated by the World Health Organization (WHO), in 2021 more than 483 million people were living with type 2 diabetes.
The number of people with diabetes has almost doubled since 1980, largely because of unhealthy eating habits, lack of physical activity and an aging population.
Knowing about the genetics of type 2 diabetes is crucial. It can help us identify people at risk of getting the disease and ways to prevent or delay it. Secondly, it can help us understand how the disease starts and progresses, and how to treat it properly.
It can also help us discover new ways to cure or reverse diabetes by focusing on the underlying genetics of the disease.
In this article, we will look at the genetics of type 2 diabetes in depth from genetics to current research.
Quick Overview:
Type 2 diabetes, a widespread health issue, is largely influenced by genetics alongside environmental factors.
It’s a polygenic disease, meaning multiple genes contribute to its risk. Key genes involved include TCF7L2, which affects insulin secretion and glucose production, and others like ABCC8 and CAPN10 which influence insulin sensitivity and glucose metabolism.
Family and twin studies show a significant hereditary component, with the risk increasing if close relatives have the condition. Understanding these genetic factors is crucial for early detection, management, and targeted treatment strategies.
For an in-depth understanding of the genetic aspects and their implications in managing type 2 diabetes, continue to read the full article.
Pathophysiology of Type 2 Diabetes?
To understand what causes type 2 diabetes, we need to explain how our bodies usually handle sugar.
When we eat, food gets broken down into sugar (or glucose) and other stuff that goes into our blood. This causes our blood sugar to rise, which makes our pancreas release something called insulin.
Insulin then attaches itself to cells all over the body, especially in our muscles, fat, and liver. This tells those cells to take up the glucose from our blood. This lowers our blood sugar and gives our cells the energy or storage they need.
In type 2 diabetes, this whole process gets messed up because of two main issues: the body’s resistance to insulin or not enough insulin in the body.
Insulin resistance is when the cells don’t respond well to insulin, and they take less glucose from the blood.
This leaves blood sugar levels high, and the pancreas has to make more insulin to try and lower them. Over time, this can lead to too much insulin in the blood (hyperinsulinemia) and the beta cells (insulin-making cells) getting tired and dying.
Not having enough insulin, or insulin deficiency, happens when the pancreas doesn’t make enough insulin to keep blood sugar levels healthy.
This can happen because the beta cells are lost or not working right. This can be due to genetics, environmental factors, or both.
Without enough insulin, glucose can’t get into the cells and ends up staying in the blood, causing high blood sugar (hyperglycemia).
The changes in type 2 diabetes can be affected by the genetics of diabetes.
For instance, some diabetes type 2 genes control how sensitive the cells are to insulin or how much insulin the pancreas can make.
Other diabetes genes control how glucose is used or stored in the cells or how it is controlled by hormones and enzymes. Some genes also control whether the beta cells live or die when under stress or damage.
By understanding how diabetes genetics affect type 2 diabetes, we can better detect, manage, and prevent this disease. We can also find new targets for therapies that can fix normal insulin function, glucose use, and the survival of beta cells.
Genetics and Type 2 Diabetes
Genetics is the study of genes, which are segments of DNA that carry instructions for making proteins – the building blocks of life. Our genes are inherited from our parents and determine many of our physical and biological characteristics, like eye color, blood type, and height.
However, it’s not only genes that influence our traits and health. Environmental factors like diet, exercise, stress and exposure to toxins can also affect how our genes work and interact with each other. This is known as gene-environment interaction.
Certain diseases happen because of changes or mutations in a single. These are called monogenic diseases, like cystic fibrosis, sickle cell anemia or monogenic diabetes (MODY).
Other diseases happen because of a mix of genetic and environmental factors that affect many genes and pathways in complex ways. These are known as polygenic or multifactorial diseases, like type 2 diabetes.
The reasons why people get type 2 diabetes can be due to their inherited genes (the genetics of diabetes) or due to their lifestyle habits like diet, physical activity, and body weight.
However, having these diabetes type 2 genes or unhealthy habits doesn’t guarantee you’ll develop the condition. It’s a complicated health issue involving many diabetes genes and how they interact with your environment.
Family Links and Twin Studies in Type 2 Diabetes
A method to figure out the role of genetics in type 2 diabetes is by observing how often it shows up in families and in twins.
Research tells us that type 2 diabetes often runs in families, indicating that if you have a parent or sibling with this condition, you’re more likely to get it too.
The risk increases with the number of family members affected and how closely related they are to you.
Another method to understand the genetic link is to compare identical twins, who share all their genes, with fraternal twins, who share half of their genes.
If type 2 diabetes were only genetic, then identical twins should always have the same diabetes status (either both have it or neither of them does), while fraternal twins should differ in their status about half the time.
But if type 2 diabetes is affected by environmental factors, identical twins might not always have the same diabetes status, and fraternal twins might show similar statuses more often than what would happen by chance.
Twin studies tell us that type 2 diabetes is partially genetic and partially environmental.
The hereditary aspect of type 2 diabetes (measuring how much genetics can explain the variation in the disease) is estimated to be between 25% and 72%, depending on the group studied and the method used.
This shows that the genetics of type 2 diabetes plays a substantial role, but it’s not the only factor.
Discovering Risky Genes
To find out which diabetes genes are involved in type 2 diabetes, scientists use different techniques, like genome-wide association studies (GWAS).
These studies scan the entire genome for variations that are more common in people with the condition than in those without it.
Since 2007, GWAS have found over 100 regions in the genome connected with the risk of type 2 diabetes.
But most of these regions have a small effect on the risk and only explain a tiny part of the hereditary nature of the disease.
Some of the genes that have been linked to type 2 diabetes are:
1. TCF7L2 gene
This gene makes a protein that helps control insulin secretion and glucose production. Changes in this gene are linked to an increased risk of type 2 diabetes in various groups.
It’s thought that about 10% of people have two copies of the high-risk variant of this gene, which boosts their risk by about 50% compared to people who do not have any copies.
2. Other notable genes
Some other genes associated with the risk of type 2 diabetes include:
- ABCC8 gene: This gene creates a protein that helps control insulin secretion by managing the opening and closing of channels that let potassium ions leave pancreatic beta cells. Variations in this gene can influence how sensitive these cells are to glucose and other signals.
- CAPN10 gene: This gene makes a protein that is involved in various cell processes, like inflammation, apoptosis (cell death), and glucose metabolism. Variations in this gene have been linked to the risk of type 2 diabetes in Mexican Americans.
- GLUT2 gene: This gene makes a protein that helps glucose move into pancreatic beta cells and liver cells. Variations in this gene can affect how much glucose these cells can sense and react to.
- GCGR gene: This gene makes a protein that is a receptor for glucagon, a hormone that raises blood glucose levels by making the liver produce more glucose. Variations in this gene can impact how the body regulates glucose levels.
Polygenic Inheritance of Type 2 Diabetes
Type 2 diabetes is a polygenic condition, meaning many genes, each with a small effect, influence it.
The more high-risk variants a person has, the higher their chance of developing the disease. However, not everyone with many high-risk variants will get type 2 diabetes, and not everyone with the condition will have many high-risk variants.
This is because factors like diet, exercise, weight, and age also impact the risk and can alter the effects of the genes.
Therefore, testing for type 2 diabetes genes isn’t very effective at predicting who will get the disease. It can only give an estimate of the relative risk based on the known variants, which may not fully capture the genetic complexity of the condition.
Furthermore, genetic testing can’t account for environmental factors that can change over time and interact with the genes.
The most effective way to prevent or delay type 2 diabetes is to lead a healthy lifestyle. This includes eating a balanced diet, being physically active, maintaining a healthy weight, and avoiding smoking.
These habits can lower the risk of type 2 diabetes even in people who have a high genetic risk. For instance, a study found that physical exercise can reduce the incidence of type 2 diabetes by 40% in people with a high genetic risk.
In a nutshell, type 2 diabetes is influenced by both genetic and environmental factors. Understanding the genetics of type 2 diabetes helps us know why some people are more prone to develop the condition.
However, making healthy lifestyle changes can significantly reduce the risk of developing type 2 diabetes, regardless of your genetic risk.
Epigenetic Relation to Type 2 Diabetes
This is a process where changes happen to our genes, but not to the actual DNA sequence. These changes can be affected by things like diet, exercise, stress, and aging.
Epigenetics can play a role in type 2 diabetes by changing how genes function, especially those that control blood sugar levels, insulin sensitivity, inflammation, and stress.
How does our environment affect the genetics of type 2 diabetes?
The environment around us also influences type 2 diabetes. Factors like pollution, our surroundings, food availability, and our social situation can interact with our genetics and affect the disease.
For example, living in areas with lots of air pollution or with limited access to healthy food can increase the risk of type 2 diabetes.
The connection between our lifestyle, our genes, and type 2 diabetes is complex and changes over time.
Physical activity and diet can affect how our genes function, and those genes can also influence how we respond to interventions designed to prevent or manage diabetes.
Genetic testing for type 2 diabetes risk?
Genetic testing looks at our DNA to see if we carry certain genetic changes associated with diseases like type 2 diabetes. This testing can be used to confirm a diagnosis, predict future risk, or guide the use of specific drugs.
With genetic testing, we can identify people who are at high genetic risk for type 2 diabetes and focus on early interventions.
It can also help personalize prevention strategies based on individual genetic profiles.
However, it’s important to remember that genetic testing has limitations and ethical implications. It doesn’t capture all the risk factors, and the results can potentially lead to privacy concerns, discrimination, and anxiety.
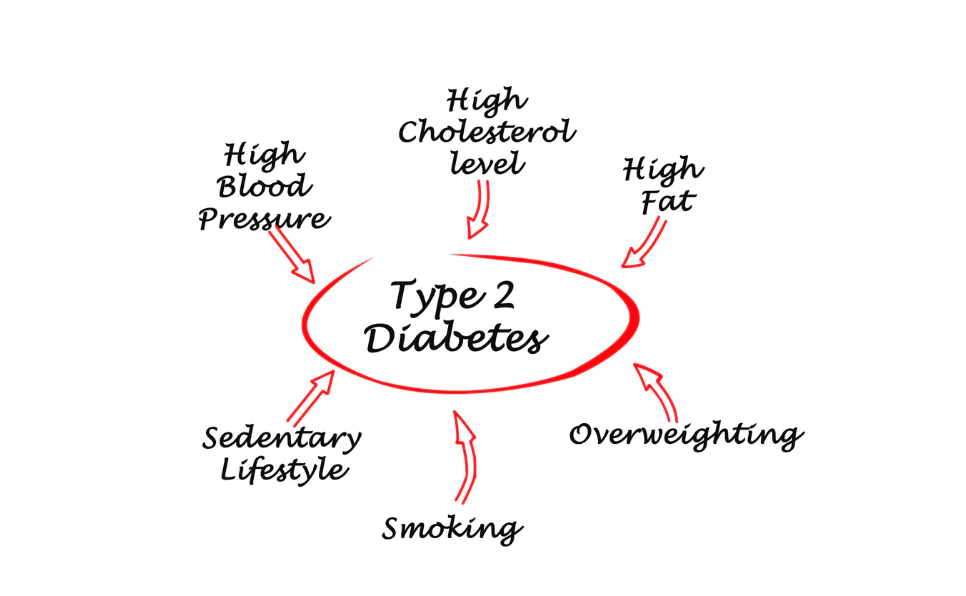
Non-Genetic Risk Factors for Type 2 Diabetes
Things other than your “diabetes genes” can increase your chances of getting type 2 diabetes.
These are called non-genetic risk factors. Even if you have the “type 2 diabetes gene” or other “diabetes genes,” these factors can push your body towards developing diabetes.
- Obesity: One of the biggest non-genetic risk factors for type 2 diabetes is being overweight or obese. Extra weight makes it harder for your body to use insulin properly. It’s like putting extra strain on a machine – eventually, it might start to break down.
- A lack of physical activity: Exercise helps your body use insulin better, so not moving around enough can make your body less able to handle sugar, even if you have the “type 2 diabetes gene.”
- Bad diet: Your diet also plays a big part. Eating too many foods high in sugar or unhealthy fats can make it harder for your body to keep your blood sugar levels stable, especially if you have “diabetes genes” that already make you more likely to get diabetes.
- Age: As we get older, our bodies might not respond to insulin as well, regardless of whether we have the “type 2 diabetes genetic” risk or not.
- Stress: It can make your body produce hormones that prevent insulin from doing its job. So, if you’re under a lot of stress, your body might struggle to keep your blood sugar levels healthy, even if you don’t have the “diabetes type 2 gene.”
Managing Type 2 Diabetes
Now, what if you already have type 2 diabetes, or you’re at risk because of your “diabetes genetics”? Don’t worry, there are ways to manage the condition and keep your body healthy.
The most important thing you can do is to maintain a healthy weight. If you’re overweight, losing even a small amount can help your body use insulin better and stabilize your blood sugar levels. This is important, even if you have the “type 2 diabetes gene”.
Regular exercise is also crucial. It helps your body use insulin more efficiently and can lower your blood sugar levels. You don’t need to run a marathon – even a brisk walk can make a difference.
Your diet also plays a big role in managing type 2 diabetes. Try to eat a balanced diet with lots of fruits, vegetables, and whole grains. Avoid foods that are high in sugar or unhealthy fats.
These simple changes can help keep your blood sugar levels stable, no matter what your “diabetes genetics” are.
Medications might also be needed to manage type 2 diabetes. Some can help your body make more insulin, some help your body use insulin better, and others can slow down how quickly your body absorbs sugar.
You should always talk to your doctor about the best treatment plan for you, especially if you have the “type 2 diabetes genetic” risk.
Managing type 2 diabetes is a lifelong commitment. Even if you have the “diabetes type 2 gene,” you can still live a healthy, active life by making some lifestyle changes and working closely with your healthcare team.
What’s next in studying the genetics of type 2 diabetes?
There’s still a lot to learn about the “diabetes genes” and the genetics of diabetes.
Future research should focus on including diverse populations in genetic studies, using new methods to identify important genes, and using this information to better predict, prevent, and treat type 2 diabetes.
The ultimate goal is precision medicine – personalized healthcare based on a person’s genetics, environment, and lifestyle.
So, in conclusion…
Type 2 diabetes is the most common form of diabetes, accounting for about 90% of all cases. It usually affects adults over the age of 45, but it can also affect younger people and children due to unhealthy eating and inactive lifestyles.
Genetics is a key part of understanding type 2 diabetes. “Is diabetes type 2 genetic?” It’s not that simple.
While our genes influence our risk of getting type 2 diabetes, our environment and lifestyle also play big roles.
Genetic testing can help predict risk and guide prevention and treatment strategies. However, the future of type 2 diabetes research lies in better understanding how our genes and environment interact, and how we can use this knowledge to better manage and treat the disease.
Ultimately, the goal is to reduce the impact of type 2 diabetes on individuals, families, and societies.
References:
- https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
- https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-2-diabetes
- https://www.nhs.uk/conditions/type-2-diabetes
- https://www.webmd.com/diabetes/qa/is-type-2-diabetes-genetic
- https://pubmed.ncbi.nlm.nih.gov/33651556
- https://www.nature.com/articles/s43586-021-00056-9
- https://pubmed.ncbi.nlm.nih.gov/29536439
- https://www.genome.gov/glossary/index.cfm?id=91
- https://diabetesjournals.org/care/article/36/5/1413/29265
- https://pubmed.ncbi.nlm.nih.gov/32674227
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5800177
- https://pubmed.ncbi.nlm.nih.gov/30603301
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6224936
- https://link.springer.com/article/10.1007/s13340-016-0299-2
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3631878
- http://world.edu/environmental-risk-factors-type-2-diabetes
- https://pubmed.ncbi.nlm.nih.gov/34792619
- https://link.springer.com/article/10.1007/s00125-021-05618-w

Dr. Sumeet is a seasoned geneticist turned wellness educator and successful financial blogger. GenesWellness.com, leverages his rich academic background and passion for sharing knowledge online to demystify the role of genetics in wellness. His work is globally published and he is quoted on top health platforms like Medical News Today, Healthline, MDLinx, Verywell Mind, NCOA, and more. Using his unique mix of genetics expertise and digital fluency, Dr. Sumeet inspires readers toward healthier, more informed lifestyles.