When we talk about Mitochondrial myopathies, they are a group of disorders that occur because of dysfunction in mitochondria – the powerhouses of our cells.
These tiny organelles are where our bodies convert food and oxygen into energy, which is vital for everything we do, from breathing to running.
Mitochondria can be affected by genetic mutations in two sets of genes – those in the mitochondrial DNA (mtDNA) and those in the nuclear DNA that relate to mitochondrial function.
Since mitochondria play a pivotal role in muscle health, any issue with their function can lead to significant health problems, including muscle weakness and neurological issues, which are hallmarks of mitochondrial myopathies.
Key Takeaways
- Mitochondrial myopathies affect everyone differently, but muscle weakness and systemic symptoms are common.
- Diagnosis involves a combination of blood tests, muscle biopsies, and genetic testing.
- Managing the condition focuses on symptom relief, lifestyle adjustments, and supportive care.
Understanding Mitochondrial Disease Myopathies
The Role of Mitochondria in the Body
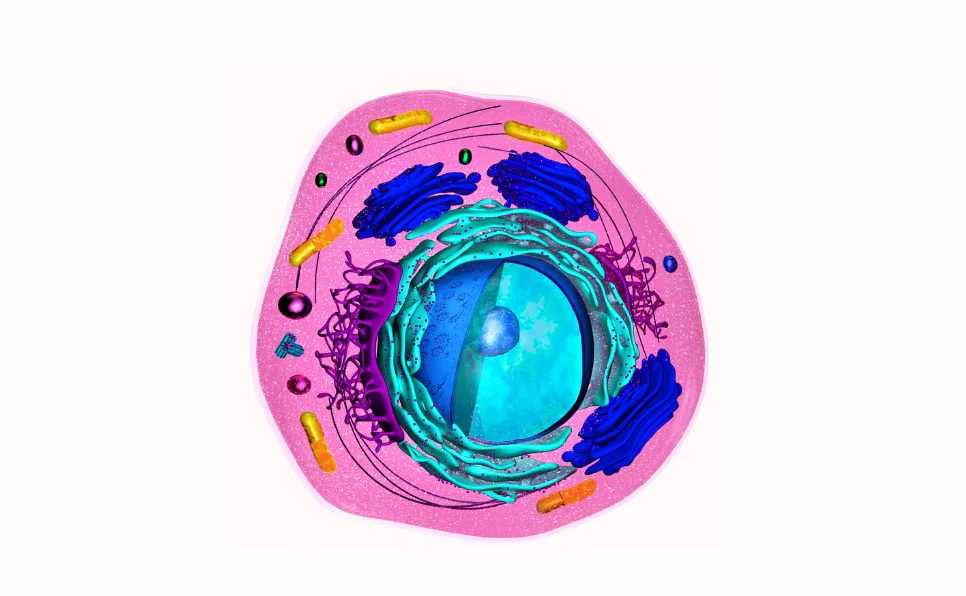
To understand mitochondrial myopathies, we need to start at the core – the role of mitochondria in our bodies.
Mitochondria do more than just produce energy; they’re involved in regulating cell death, cell growth, and the cellular response to stress.
Their main job, though, is to convert the energy from food into a form that cells can use, a process known as oxidative phosphorylation.
It’s a complex process involving many steps and components, all of which need to work perfectly. When they don’t, that’s when problems arise.
Mitochondria’s unique genetic characteristics also play into this. They have their own DNA, which is passed down from mothers to their children.
This mtDNA is more prone to mutations than nuclear DNA, partly because it has less efficient repair mechanisms. These mutations can disrupt the normal functioning of mitochondria and lead to mitochondrial diseases.
What Causes Mitochondrial Myopathies?
The root cause of mitochondrial myopathies lies in genetic mutations that affect how mitochondria function.
These mutations can be in the mtDNA or in the nuclear DNA that codes for mitochondrial components.
Because mitochondria are present in every cell type except red blood cells, mutations in mitochondrial genes can affect multiple systems in the body, but the most noticeable effects are often in organs and tissues that require a lot of energy, like muscles and the brain.
The inheritance patterns of these disorders can be complicated. Mutations in mtDNA follow a maternal inheritance pattern, meaning they can only be passed from mother to offspring, not from father to offspring.
On the other hand, mutations in nuclear DNA follow the regular patterns of inheritance (autosomal dominant, autosomal recessive, or X-linked), which means they can come from either parent and affect both males and females.
Types of Mitochondrial Myopathies
Mitochondrial disease myopathies come in various forms, each with its own set of symptoms and challenges. Here are a few:
- Kearns-Sayre Syndrome (KSS): This rare condition typically starts before the age of 20 and involves progressive external ophthalmoplegia (PEO), which means weakness in the eye muscles, leading to drooping eyelids and difficulty moving the eyes. Besides eye problems, KSS can cause heart block, which might need a pacemaker and problems with coordination and balance (ataxia). It’s a bit of a mixed bag in terms of symptoms, affecting various parts of the body differently.
- MELAS (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes): The name might be a mouthful, but it highlights the main features of this condition. MELAS often starts in childhood and leads to muscle weakness and pain, recurrent headaches, loss of appetite, and seizures. The “stroke-like episodes” don’t always result in full strokes but can severely affect movement and cognition. It’s a challenging condition because of how unpredictable and varied the symptoms can be.
- MERRF (Myoclonic Epilepsy with Ragged Red Fibers): This type gets its name from the appearance of muscle cells under a microscope; they have “ragged red fibers,” which are abnormal mitochondria that clump together. People with MERRF often experience myoclonic epilepsy, which involves quick, involuntary muscle jerks. Besides epilepsy, individuals may face muscle weakness, coordination issues, and sometimes hearing loss and heart problems. It’s a lot for anyone to manage, and the unpredictability adds an extra layer of difficulty.
There are other types of mitochondrial myopathies, each with its own unique set of symptoms and genetic causes.
For example, Pearson syndrome affects the bone marrow and pancreas, leading to severe anemia and failure to thrive in infants.
Another, LHON (Leber’s Hereditary Optic Neuropathy), leads to sudden vision loss in young adults.
These conditions highlight the diversity of mitochondrial myopathies and the wide-ranging impact they can have on individuals and families.
What they all share, however, is the underlying issue of mitochondrial dysfunction leading to energy production problems.
Symptoms and Diagnosis Of Mitochondrial Myopathies
When it comes to mitochondrial disease myopathies, the symptoms can be as diverse as the people who experience them. Heteroplasmy can further lead to variability in the phenotype.
The main hallmark, though, involves muscle weakness and a pronounced difficulty in performing tasks that require physical endurance. This isn’t just feeling tired after a workout; it’s an overwhelming fatigue that doesn’t go away with rest.
But it’s not all about the muscles. Mitochondrial myopathies can affect almost any system in the body, leading to a wide range of neurological and systemic symptoms.
These can include but are not limited to:
- Muscle weakness and exercise intolerance: The feeling of exhaustion doesn’t match the level of activity.
- Neurological symptoms: Issues like seizures, learning disabilities, and developmental delays can occur.
- Systemic symptoms: This could mean anything from heart problems to diabetes, digestive issues, and more.
It’s a mixed bag because mitochondria are everywhere in your body, powering every cell. When they’re not working right, the effects can be widespread.
Diagnostic Approaches
Getting to the bottom of mitochondrial disease myopathies involves a few steps. Here’s a rundown:
- Blood tests and imaging: These can show elevated levels of certain enzymes or abnormalities in the brain or muscles.
- Muscle biopsy: A small sample of muscle tissue can reveal characteristic ragged red fibers, a tell-tale sign of some mitochondrial disorders.
- Genetic testing: Since many mitochondrial myopathies are passed down through families, genetic tests can confirm a diagnosis and help with family planning.
Diagnosing these conditions can be complex because symptoms overlap with many other diseases.
Managing and Treating Mitochondrial Myopathies
Current Treatment Options
There’s no cure for mitochondrial myopathies yet. But that doesn’t mean there’s nothing you can do.
Treatment mainly focuses on managing symptoms and improving quality of life. Here’s what’s on the table:
- Medications and supplements: Some meds can help manage symptoms like muscle pain and seizures. Supplements like CoQ10 might improve energy levels, but evidence varies.
- Physical therapy and exercise: Staying active within your limits can help maintain muscle strength and function.
Lifestyle Adjustments and Support
Adjusting to life with mitochondrial myopathy is a personal journey, but here are some strategies that can help:
- Nutrition and diet: There’s no one-size-fits-all diet, but eating balanced meals and staying hydrated can support overall health.
- Support groups and counseling: Connecting with others who understand can be a huge relief. Mental health support is also key.
Advances in Treatment Research
Science is always moving, and there are some exciting areas of research for mitochondrial myopathies:
- Gene therapy and mitochondrial replacement therapy: These are cutting-edge approaches aiming to fix the underlying genetic problems.
- Ongoing clinical trials: New treatments are being tested all the time, offering hope for better management options in the future.
- New diagnostic techniques: Advances in genetic testing make diagnosis faster and more accurate.
- Personalized medicine approaches: Treatments tailored to an individual’s genetic makeup are on the horizon, promising more effective care.
Final Thoughts
Mitochondrial myopathies can be daunting, but understanding the condition and knowing how to manage it can make a big difference.
Advances in research offer hope for the future, and support from healthcare providers, family, and community can provide strength for the journey.
FAQs
What is the life expectancy for someone with a mitochondrial myopathy?
Life expectancy varies widely among individuals with mitochondrial myopathies, depending on the type and severity. Some live normal lifespans with management, while others may have more serious complications.
Can mitochondrial myopathies be cured?
Currently, there is no cure for mitochondrial disease myopathies. Treatment focuses on managing symptoms and improving quality of life through medications, physical therapy, and lifestyle adjustments.
How can genetic counseling help families affected by mitochondrial myopathies?
Genetic counseling provides families with information on inheritance patterns, risks to other family members, and implications for future pregnancies, supporting informed decisions about family planning and care.
Are there any dietary recommendations for individuals with mitochondrial myopathies?
While there’s no one-size-fits-all diet, maintaining balanced nutrition and hydration is crucial. Some may benefit from specific supplements like CoQ10, but consultation with a healthcare provider is recommended.
How do mitochondrial disease myopathies affect pregnancy and childbirth?
Mitochondrial myopathies can increase risks during pregnancy and childbirth, requiring close monitoring by a healthcare team. Effects vary widely and depend on the condition’s severity and type.
What are the latest advancements in the treatment of mitochondrial myopathies?
Recent advancements include research into gene therapy, mitochondrial replacement therapy, and personalized medicine approaches aimed at targeting the underlying genetic causes of the disease.
How can technology aid in the daily management of mitochondrial myopathies?
Technology, such as wearable devices and mobile apps, can help track symptoms, manage medication schedules, and facilitate communication with healthcare providers, enhancing daily management and care.
For Further Reading:
- Understanding mitochondrial myopathies: a review – PeerJ
- Diagnosis and Treatment of Mitochondrial Myopathies – Neurotherapeutics
- Advances in Primary Mitochondrial Myopathies (PMM) – Current Open Neurol
- Current and Emerging Clinical Treatment in Mitochondrial Disease – Molecular diagnosis and therapy
- A clinical approach to diagnosis and management of mitochondrial myopathies – Neurotherapeutics
- Mitochondrial Disease: Advances in clinical diagnosis, management, and pathogenesis – Current Gent Med Rep

Dr. Sumeet is a seasoned geneticist turned wellness educator and successful financial blogger. GenesWellness.com, leverages his rich academic background and passion for sharing knowledge online to demystify the role of genetics in wellness. His work is globally published and he is quoted on top health platforms like Medical News Today, Healthline, MDLinx, Verywell Mind, NCOA, and more. Using his unique mix of genetics expertise and digital fluency, Dr. Sumeet inspires readers toward healthier, more informed lifestyles.