Mitochondrial Replacement Therapy (MRT) or Mitochondrial donation is one of those scientific advancements that sounds like it’s straight out of a science fiction novel. Yet, it’s a real and groundbreaking medical procedure aimed at preventing some serious genetic disorders.
At its core, MRT involves replacing faulty mitochondria (the parts of our cells that generate energy) with healthy ones from a donor to prevent mitochondrial diseases from being passed from mother to child.
It’s a bit like replacing the batteries in a device to ensure it works properly. But, as with any groundbreaking technology, it comes wrapped in a bundle of ethical questions and considerations.
Why fuss over the ethics, you might wonder? Well, we’re tinkering with the very blueprint of life here, and that comes with its share of risks, uncertainties, and moral dilemmas.
The goal of this article isn’t just to throw hard-to-digest scientific facts at you. Instead, I’m here to break down what MRT is, how it works, and why the ethical debate surrounding it is both necessary and complex.
Understanding Mitochondrial Donation
What is Mitochondrial Replacement Therapy?
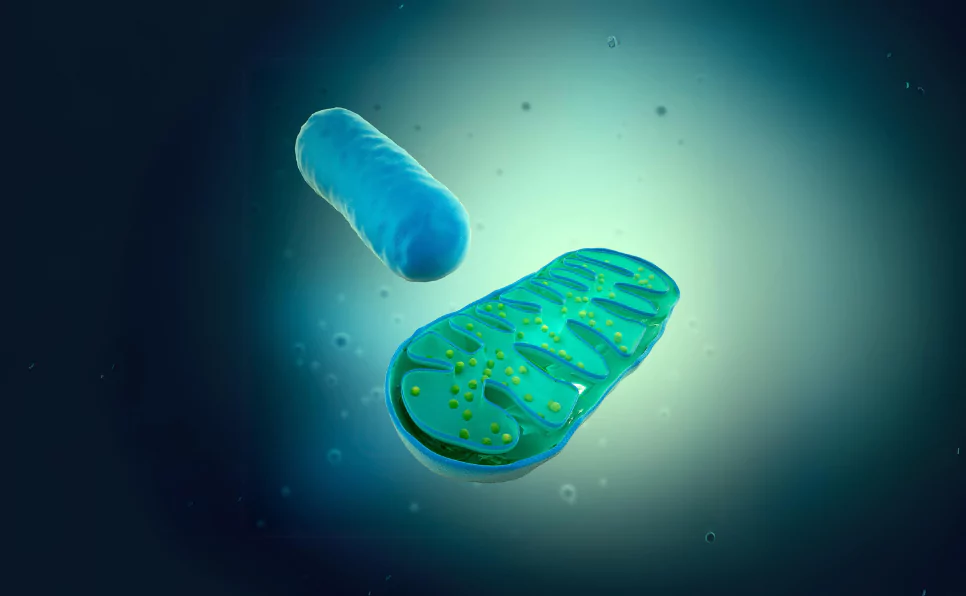
Let’s start with the basics. Imagine every cell in your body as a tiny factory.
The mitochondria are the power stations of these factories, producing the energy needed for the cell to function. But sometimes, these power stations have defects a.k.a. mutations, leading to mitochondrial diseases – conditions that can be severe and are currently incurable.
Enter MRT. This technique aims to replace the faulty mitochondria in a mother’s egg with healthy mitochondria from a donor’s egg.
The result? The baby inherits the genetic information of its parents but uses the energy-producing capabilities of the donor’s mitochondria.
Think of it as a cellular-level baton pass in a relay race, ensuring the next runner (or in this case, the newborn) gets a healthy start.
How it’s done involves a bit of scientific finesse.
There are mainly two techniques: one involves transferring the nuclear DNA from one egg or embryo to another, leaving behind the defective mitochondria. The other technique mixes the contents of the donor and the parent’s eggs before fertilization.
Both methods aim to ensure the resulting child is free of mitochondrial disease.
The Purpose of MRT
The concept of this therapy comes from the fact that mtDNA is inherited from mothers to kids. When the egg and sperm fuse to create the child, mitochondrial DNA is only present in the egg at the time of fusion.
So, kids get all their mtDNA from the mother.
MRT therapy involves replacing the mitochondria of the egg with an egg from another healthy donor before fusion with the sperm.
The primary goal here is clear: to prevent the transmission of mitochondrial diseases from mother to child.
These diseases can be debilitating and life-threatening, affecting the brain, muscles, heart, and other critical systems.
By replacing faulty mitochondria, MRT offers hope for families plagued by these genetic conditions.
But the benefits might stretch beyond just the immediate family. MRT has the potential to break the cycle of mitochondrial diseases, reducing the overall incidence in the population over time.
It’s about giving children a chance at a healthy life, free from conditions that currently have no cure.
From a personal perspective, as someone deeply entrenched in the world of genetics, the promise of MRT is thrilling.
It’s a testament to how far we’ve come in understanding the complexities of human biology. But it’s also a reminder of our responsibility to navigate these advancements carefully, with a keen eye on the ethical implications.
In essence, MRT is not just about preventing disease. It’s about opening new doors in the world of genetic medicine, offering hope where there was previously none.
However, as we march forward, it’s crucial to balance our enthusiasm for scientific progress with a thoughtful consideration of the ethical, social, and moral questions it brings to the table.
Ethical Considerations of MRT
The journey into the world of MRT is not just a scientific adventure but also an ethical dilemma. As we go into the nuances of this therapy, it’s crucial to recognize the delicate balance between innovation and the moral questions it raises.
The Genetic Modification Debate
At the heart of MRT’s ethical questions is the act of modifying the germline, essentially, making changes that can be passed down to future generations.
This aspect of MRT sets it apart from other medical interventions. The implications are profound, stirring concerns over potential unforeseen consequences, ethical boundaries, and the essence of human inheritance.
Critics argue that germline modification could lead to unforeseen genetic issues, disrupt the natural evolutionary process, or even pave the way for ‘designer babies.’
Supporters, however, see it as a beacon of hope for eradicating debilitating mitochondrial diseases, arguing that the benefits far outweigh the theoretical risks.
Comparing MRT to other forms of genetic modification, such as CRISPR/Cas9 used in somatic cell therapy, highlights a significant ethical divide.
While somatic modifications affect only the individual and not their offspring, MRT’s alterations to the mitochondrial DNA will be passed on, marking a fundamental shift in our approach to genetic inheritance.
The Concept of “Three-Parent” Babies
The term “three-parent babies” often evokes a mix of fascination and apprehension.
In reality, it oversimplifies and somewhat misrepresents the process.
MRT involves replacing faulty mitochondrial DNA (mtDNA) from a mother’s egg with healthy mtDNA from a donor egg, in addition to the nuclear DNA from the mother and father.
This means the baby inherits genetic material from three people, though with the vast majority coming from the parents.
With this, there’s an undercurrent of worry about the child’s identity and potential stigmatization. Yet, from a scientific and ethical standpoint, the focus remains on the profound potential to prevent life-threatening diseases, framing the debate within a context of medical necessity versus societal norms.
Consent and Autonomy
In the world of genetic therapies, informed consent is a cornerstone. However, MRT introduces complex challenges, particularly concerning the autonomy and rights of the future child. How do we navigate consent when the individual most affected by the decision has no voice in the matter?
This dilemma isn’t unique to MRT but is magnified by its implications for future generations. The debate centers on whether the potential to prevent mitochondrial diseases justifies the intervention before an individual’s existence.
It’s a profound ethical puzzle, balancing parental desires against the child’s right to an unmodified genetic lineage.
Access and Equity
MRT’s promise also raises questions about access and equity.
Currently, the therapy’s availability is limited, often restricted to countries with advanced medical research facilities and regulatory frameworks that permit such procedures.
This disparity creates a risk of exacerbating global health inequities, potentially giving rise to a ‘genetic underclass’, individuals who, due to socioeconomic constraints, cannot access these life-altering treatments.
The challenge lies in ensuring equitable access to MRT, transcending borders and economic barriers. It’s an ethical imperative to democratize access to such therapies, ensuring that the benefits of scientific advancements are shared broadly, rather than concentrated among a privileged few.
Legal and Regulatory Landscape
Navigating the legal and regulatory terrain of MRT is akin to charting a course through uncharted waters. The approach varies significantly across the globe, reflecting diverse ethical, cultural, and legal perspectives.
Current Legal Status of MRT Worldwide
At the time of writing this, only a handful of countries have ventured to legalize MRT, each with its unique regulatory framework.
The UK, for example, stands at the forefront, having established a rigorous vetting process for MRT applications. This careful, case-by-case approach balances the technology’s potential benefits with ethical and safety considerations.
Elsewhere, the legal status of MRT remains in flux, with many countries still grappling with the ethical implications and how best to regulate such therapies.
The variance in legal stances underscores the global community’s cautious approach to germline modification and its potential repercussions.
International Guidelines and Standards
The international community has made efforts to establish guidelines and standards for MRT and other genetic therapies.
Organizations like the World Health Organization (WHO) and the International Society for Stem Cell Research (ISSCR) play pivotal roles in this endeavor, aiming to foster a consensus on ethical practices and safety standards.
Yet, achieving global agreement is challenging, given the wide array of cultural, ethical, and legal perspectives on genetic modification.
The ongoing dialogue among scientists, ethicists, policymakers, and the public is crucial for navigating these complex issues.
Final Thoughts
MRT embodies both the incredible promise of genetic science and the profound ethical dilemmas it engenders.
The ethical considerations, spanning the genetic modification debate, the concept of “three-parent” babies, issues of consent and autonomy, and concerns about access and equity, underscore the complexity of integrating such therapies into our medical and societal frameworks.
The future outlook for MRT and genetic therapies hinges on our ability to balance innovation with ethical responsibility, ensuring that such advancements serve the greater good without compromising our values or the well-being of future generations.
FAQs
Can MRT be used for conditions other than mitochondrial diseases?
Currently, MRT is specifically designed to prevent the transmission of mitochondrial diseases from mother to child. Its application beyond this scope, such as treating other genetic conditions, remains under research and is not yet a practical or approved use.
What are the long-term health implications for children born using MRT?
The long-term health implications for children born via MRT are still being studied. Early outcomes are promising, indicating normal development. However, ongoing research is crucial to fully understand any potential long-term effects of having DNA from three individuals.
How does MRT differ from traditional IVF treatments?
MRT differs from traditional IVF by incorporating a third set of mitochondrial DNA (mtDNA) to prevent certain genetic diseases. While IVF involves fertilizing an egg with sperm in a lab, MRT adds the step of replacing faulty mitochondrial DNA to ensure the child doesn’t inherit mitochondrial disorders.
Are there alternatives to MRT for preventing mitochondrial diseases?
Alternatives to MRT include pre-implantation genetic diagnosis (PGD) during IVF to select embryos free of mitochondrial disorders. However, PGD cannot eliminate the risk as completely as MRT, which offers a unique solution for women at high risk of passing on mitochondrial diseases.
How are ethical considerations of MRT being addressed in research and clinical trials?
Ethical considerations are central to MRT research and clinical trials. Regulatory bodies and ethics committees rigorously review each case, focusing on consent, the welfare of the child, and long-term impacts. Public and expert dialogues continually shape the ethical framework surrounding MRT.
For Further Reading
- Progress in mitochondrial replacement therapies. Nature Reviews Molecular Cell Biology
- Pronuclear transfer in human embryos to prevent transmission of mitochondrial DNA disease. Nature.
- Mitochondrial gene replacement in primate offspring and embryonic stem cells. Nature.
- Mitochondrial replacement in human oocytes carrying pathogenic mitochondrial DNA mutations. Nature.
- Live birth derived from oocyte spindle transfer to prevent mitochondrial disease. Reproductive Biomedicine Online.
- Three-parent in vitro fertilization: Gene replacement for the prevention of inherited mitochondrial diseases. Fertility and Sterility.
- Towards clinical application of pronuclear transfer to prevent mitochondrial DNA disease. Nature.
- Mitochondrial replacement therapy in reproductive medicine. Trends in Molecular Medicine

Dr. Sumeet is a seasoned geneticist turned wellness educator and successful financial blogger. GenesWellness.com, leverages his rich academic background and passion for sharing knowledge online to demystify the role of genetics in wellness. His work is globally published and he is quoted on top health platforms like Medical News Today, Healthline, MDLinx, Verywell Mind, NCOA, and more. Using his unique mix of genetics expertise and digital fluency, Dr. Sumeet inspires readers toward healthier, more informed lifestyles.