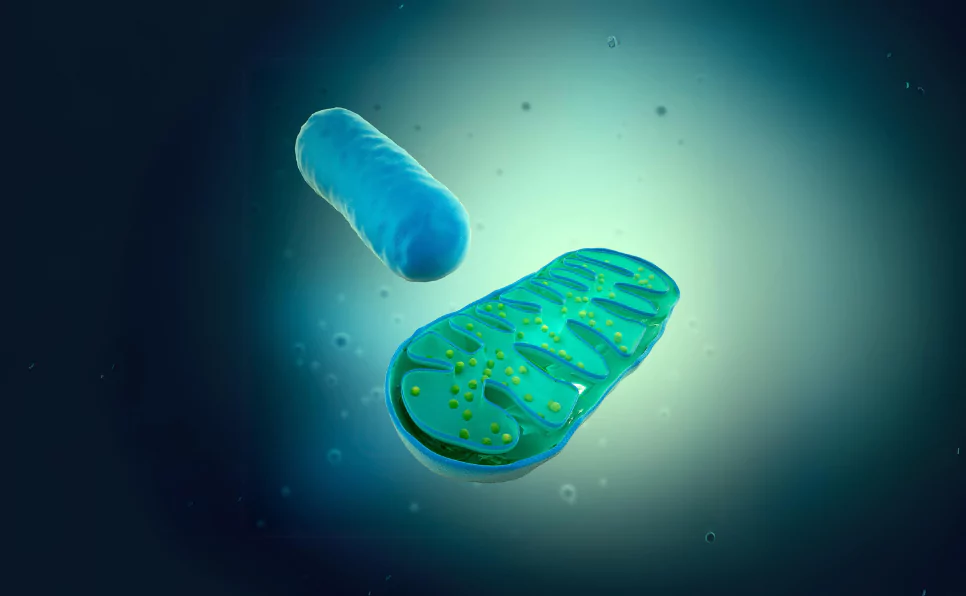
Mitochondria are like tiny factories inside our cells, churning out energy in the form of ATP (adenosine triphosphate), which is the currency our bodies use for every single action, from breathing to running marathons.
But what happens when these powerhouses malfunction?
This is where mitochondrial diseases come into play. They are a group of disorders caused by dysfunction in the mitochondria.
The significance of these diseases goes beyond energy production failure; they can affect almost any part of the body, including the brain, muscles, heart, and liver.
Mitochondrial diseases are complex, partly because mitochondria are involved in so many different functions within our cells.
Key Takeaways
- Mitochondrial diseases disrupt energy production, affecting the brain, muscles, heart, and liver.
- Mitochondria do more than make energy. They control cell death, cell communication, and cell growth.
- These diseases are often genetic, coming from mtDNA mutations. Symptoms include muscle weakness and neurological issues.
- Treatments aim to manage symptoms. Strategies include diet, exercise, and customized care plans. Research into gene therapy and mitochondrial replacement offers hope.
The Role of Mitochondria in Health
Mitochondria produce energy through a process called oxidative phosphorylation. This might sound complicated, but it’s essentially a complex chain of reactions where nutrients from our food are converted into ATP.
Without enough ATP, our cells can’t function properly, leading to the symptoms of mitochondrial diseases. But energy production is just the start.
Beyond Energy Production
Mitochondria also play crucial roles in regulating cell death (apoptosis), signaling between cells, and even the growth of new cells.
This means they’re not just energy factories; they’re involved in making sure cells behave as they should, die when they’re supposed to, and communicate effectively with each other.
These roles are vital for maintaining health, aging, and responding to disease.
Understanding Mitochondrial Diseases
What Causes Mitochondrial Diseases?
Most mitochondrial diseases are genetic. They can be caused by mutations in the DNA that makes up the mitochondria (mtDNA) or in the nuclear DNA that affects mitochondrial function.
Inherited mutations are passed down from parents (mother) to children, while spontaneous mutations happen by chance.
Mitochondrial DNA is inherited only from the mother, which adds another layer of complexity to how these diseases are passed on in families.
Types of Mitochondrial Diseases
Mitochondrial diseases are a diverse group, each with its unique set of challenges. While there are many, let’s dive a bit deeper into a few notable ones to get a sense of their impact.
MELAS (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like Episodes):
This condition is a bit of a mouthful, isn’t it? MELAS primarily impacts the brain and muscles.
Individuals with MELAS often experience muscle weakness, headaches, seizures, and even stroke-like episodes that aren’t caused by traditional strokes.
These episodes can lead to loss of consciousness or altered consciousness, and over time, they can result in cognitive decline or neurological issues.
The “lactic acidosis” part refers to a buildup of lactic acid in the body, which can cause additional symptoms like nausea and fatigue.
Leber’s Hereditary Optic Neuropathy (LHON):
LHON is another mitochondrial disease that strikes differently.
It typically leads to sudden vision loss in one eye, followed by the other, potentially leading to legal blindness.
This vision loss is due to the death of cells in the optic nerve, which is crucial for vision.
Unlike MELAS, LHON’s primary symptom is vision-related, though it can sometimes be accompanied by other issues like muscle weakness or cardiac symptoms.
But these two are just the tip of the iceberg. There are others, like:
Kearns-Sayre Syndrome (KSS): KSS shows up by the age of 20, bringing with it symptoms like droopy eyelids (ptosis), problems with the retina that can lead to vision loss, and heart issues. People with KSS might also struggle with coordination and balance.
Mitochondrial DNA Depletion Syndrome (MDS): MDS is a serious condition where there’s a significant reduction in mitochondrial DNA in affected tissues. This can lead to muscle weakness, neurological issues, or liver failure, depending on which tissues are impacted.
Myoclonic Epilepsy with Ragged Red Fibers (MERRF): The name comes from the appearance of muscle cells under a microscope, they look ragged and stained red. Symptoms include muscle twitches (myoclonus), seizures, muscle weakness, and in some cases, hearing loss or cognitive issues.
Understanding these conditions is crucial, not just for those affected and their families, but for researchers and healthcare providers striving to find better treatments and, hopefully, cures.
Symptoms and Diagnosis
Each mitochondrial disease has its own set of symptoms, which can range from mild to severe.
They can appear at any age, from infancy through adulthood, making diagnosis and treatment a tailored process.
Symptoms can vary widely but often include muscle weakness, neurological problems, stroke-like episodes, and more. Because these symptoms can overlap with many other conditions, diagnosis can be challenging.
One important aspect of mitochondrial genetics is the concept of homoplasmy and heteroplasmy, which significantly impacts the presentation and severity of mitochondrial diseases.
In a state of homoplasmy, all mitochondria within a cell have the same DNA, either all normal or all mutated.
In contrast, heteroplasmy refers to a mixture of mitochondria with normal and mutated DNA within the same cell.
The proportion of mutated mitochondria in heteroplasmic individuals can vary widely, influencing the onset and severity of disease symptoms.
This variability can lead to a broad spectrum of disease manifestations, even within the same family, complicating diagnosis and treatment strategies.
Diagnostic methods include genetic testing, which can identify mutations in mitochondrial or nuclear DNA, and muscle biopsies, which can show abnormalities in muscle cells.
These tests are crucial for getting a correct diagnosis and understanding the specific type of mitochondrial disease a person has.
Living with Mitochondrial Diseases
Living with mitochondrial diseases presents unique challenges and requires a nuanced approach to management and care.
These diseases can affect every aspect of a person’s life, from their energy levels to their physical and mental health. Yet, with the right strategies, individuals and families can navigate these challenges more effectively.
Managing Symptoms
Mitochondrial diseases come with a wide range of symptoms, which can vary greatly from person to person.
Common symptoms include muscle weakness, neurological problems, cardiac and respiratory issues, and extreme fatigue.
Since these diseases are currently incurable, treatment focuses on managing symptoms and improving quality of life.
Nutritional Support:
Proper nutrition is crucial. Some patients might benefit from specific diets or supplements that can help optimize mitochondrial function.
For example, a diet high in fats and low in carbohydrates, known as the ketogenic diet, has been shown to be beneficial for some individuals with mitochondrial diseases.
However, there’s no one-size-fits-all solution, and dietary plans should be tailored to each individual’s needs.
Exercise:
Regular, moderate exercise can also play a key role in managing symptoms.
Exercise has been shown to improve mitochondrial function in some individuals. However, it’s important to balance activity levels with energy limitations.
Physical therapy can be beneficial, helping to maintain muscle strength without overexertion.
Personalized Care Plans:
Perhaps most importantly, each treatment plan must be personalized. What works for one person may not work for another.
Regular check-ups with healthcare providers who are knowledgeable about mitochondrial diseases are essential.
Together, patients and doctors can craft a care plan that addresses the specific constellation of symptoms each individual faces.
The Role of Genetic Counseling
Genetic counseling is an invaluable resource for families affected by mitochondrial diseases.
These conditions are often inherited, which means understanding the genetic risks and implications is crucial for current and future family planning.
Genetic counselors can provide detailed information about how mitochondrial diseases are passed down through families, which can be complex due to the unique inheritance patterns of mitochondrial DNA.
They can also offer insights into the likelihood of a disease manifesting in future generations and discuss testing options for family members.
For families facing a new diagnosis, genetic counselors can be a source of support, helping them to navigate the emotional and practical challenges of living with a mitochondrial disease.
Advances in Research and Treatment
Despite the challenges that come with mitochondrial diseases, there is hope on the horizon.
The field of mitochondrial medicine is advancing rapidly, with research efforts focused on developing more effective treatments and, ultimately, cures.
Current Research Directions
Gene Therapy: One promising area of research is gene therapy. Scientists are exploring ways to repair or replace defective mitochondrial genes with healthy ones.
While still in the early stages, some gene therapy approaches have shown success in laboratory settings, offering hope for future treatments.
Mitochondrial Replacement Therapy (MRT): Another innovative approach is mitochondrial replacement therapy, which involves creating an embryo with healthy mitochondria donated by a third party.
This technique could prevent the transmission of mitochondrial diseases from mother to child. MRT has sparked ethical and regulatory debates, but it represents a significant step forward in preventing these diseases.
Final Words
Mitochondrial diseases are complex conditions that disrupt our cells’ ability to produce energy, affecting nearly every aspect of the body’s functioning.
From the brain and muscles to the heart and liver, these diseases present unique challenges for those affected.
Treatment today focuses on managing symptoms to improve quality of life, requiring a tailored approach that includes nutritional support, appropriate exercise, and regular medical care.
Understanding and addressing these diseases is critical not just for patients and families but for advancing medical science toward effective treatments and potential cures.
For Further Reading:
- The mitochondrial proteome and human disease – Annual Review of Genomics and Human Genetics
- Supercomplex assembly determines electron flux in the mitochondrial electron transport chain – Science
- Sequence and organization of the human mitochondrial genome – Nature
- Monogenic mitochondrial disorders – New England Journal of Medicine
- Mitochondrial disorders overview – GeneReviews®
- Mitochondrial diseases – Nature Reviews Disease Primers
- Loss-of-function mutations in MGME1 impair mtDNA replication and cause multisystemic mitochondrial disease – Nature Genetics

Dr. Heena Arora, a passionate geneticist and microbiologist, is a valuable asset to the Genes Wellness team. Her seminal work includes identifying a key gene for white rust resistance in mustard. Leveraging her deep expertise in genetics and microbiology, she ensures the accuracy and integrity of our content. Dr. Heena’s commitment to knowledge dissemination makes her an integral part of our team.