Sickle cell disease, often known as SCD, is an inherited illness that affects the shape and function of the red blood cells that carry oxygen around our body. It’s a worldwide problem, touching many lives, especially those with African, Asian, Middle Eastern, and Mediterranean roots.
The disease can cause severe pain, anemia, infections, organ damage, and in the worst cases, even death. There hasn’t been a definitive cure for sickle cell disease, and the existing treatment options often have side effects.
Therefore, finding a better way to treat SCD, potentially a sickle cell anemia cure, has become a big health challenge globally.
One potential method being looked at is gene therapy for sickle cell disease. This treatment modifies the very genes causing SCD. The goal is to fix the problematic hemoglobin gene or to introduce a new gene that makes normal hemoglobin.
This kind of sickle cell disease gene therapy could be a long-lasting or permanent solution for SCD patients. However, gene therapy for sickle cell disease also has many challenges, including technical, ethical, and regulatory ones, that need to be overcome for it to be safe and widely available.
In this article, we’ll dig deeper into:
- What triggers SCD genetically and how does it affect the body?
- What symptoms and complications are associated with SCD, and how are they currently managed?
- How does gene therapy work as a cure for sickle cell, and what are the different types?
- What are the potential benefits and risks of using gene therapy for curing sickle cell anemia and what does the future hold?
Understanding Sickle Cell Disease
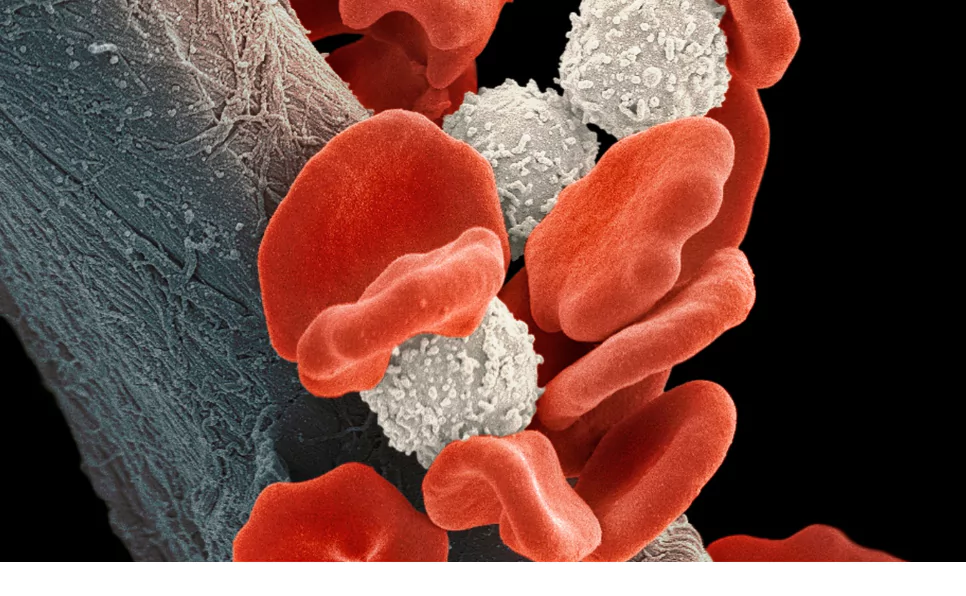
Normal hemoglobin is made up of four parts: two alpha-globins and two beta-globins. In the case of SCD, a tiny change in the beta-globin part causes a huge shift in hemoglobin’s structure and function.
This altered hemoglobin, known as hemoglobin S (HbS), tends to form long chains when it loses oxygen. These chains change the red blood cells from being round and flexible to a rigid, sickle shape.
The sickle cells also stick together, creating blockages in small blood vessels. This reduces the oxygen supply to different tissues and organs, leading to damage and inflammation.
Genetics of Sickle Cell Anemia
Sickle cell Disease is a genetic condition resulting from mutations in the HBB gene, which provides instructions for making a part of hemoglobin. This mutation leads to the production of abnormal hemoglobin, causing red blood cells to assume a sickle shape that obstructs blood flow and reduces oxygen delivery.
Is Sickle Cell Disease Inherited?
Sickle cell disease (SCD) is inherited in an autosomal recessive manner, meaning a child must receive one mutated HBB gene from each parent to develop the disease. Individuals with just one faulty gene are considered carriers with the sickle cell trait, typically without SCD symptoms, but they can pass the mutation to their offspring
Symptoms of SCD
The signs and complications of SCD can change over time and differ between individuals. Common signs and symptoms include:
- Anemia: This condition results in a low number of red blood cells or hemoglobin in the blood, leading to fatigue, weakness, breathlessness, dizziness, and pale skin. Anemia in SCD happens due to the rapid breakdown of sickle cells and a reduced production of new red blood cells.
- Pain crises: These are episodes of severe pain when sickle cells block blood flow to parts like the chest, abdomen, joints, bones, or muscles. The pain can last for hours to days and can be triggered by factors like infection, dehydration, stress, temperature changes, or high altitude. Pain crises can affect daily activities and quality of life.
- Infections: People with SCD are more prone to infections because sickle cells can damage the spleen, an organ that helps fight infections. They are also more likely to get infections from certain bacteria that can cause pneumonia or meningitis. To prevent infections, people with SCD need to regularly receive vaccinations and antibiotics.
- Organ damage: This can occur due to low oxygen supply or repeated episodes of lack of blood flow caused by sickle cells. Some of the organs that can be affected include the brain, heart, lungs, kidneys, liver, eyes, and skin.
- Growth and development: Children with SCD can experience delayed growth or development due to anemia, infections, organ damage, or poor nutrition. They may also experience delayed puberty or reduced fertility.
Management of SCD
The existing treatment strategies for SCD aim to prevent or manage the disease’s symptoms and complications. Some of the common treatments include:
- Pain medication: Drugs like nonsteroidal anti-inflammatory drugs, opioids, or adjuvant drugs can help manage pain during a crisis or chronic pain. However, these medications can also have side effects like addiction, constipation, nausea, or liver damage.
- Blood transfusions: This involves receiving healthy red blood cells from a donor to increase the blood’s oxygen-carrying capacity and reduce the proportion of sickle cells. This can help prevent or treat complications like stroke, acute chest syndrome, or severe anemia. However, it also carries risks like infection, allergic reaction, iron overload, or alloimmunization (development of antibodies against donor blood cells).
- Hydroxyurea: This medication stimulates the production of fetal hemoglobin (HbF), a type of hemoglobin that prevents the polymerization of HbS and reduces the sickling of red blood cells. Hydroxyurea can help reduce the frequency and severity of pain crises and acute chest syndrome and improve survival in adults with SCD. However, it can also have side effects like bone marrow suppression, increased risk of infection, skin ulcers, or cancer.
Gene Therapy For SCD: The Game-Changing Strategy
Gene therapy is a modern medical method used to alter a person’s genes to fix or cure diseases. Genes are the building blocks of our body that give cells instructions to make proteins. These proteins are necessary for our body to function properly. But sometimes, these genes can have mistakes that lead to diseases. Gene therapy aims to fix these mistakes by swapping, turning off, or inserting new or improved genes into the cells.

One of the diseases that gene therapy has great potential to treat is sickle cell disease. It is caused by a mutation in the gene responsible for making hemoglobin, the protein that carries oxygen in our blood cells.
The cure for sickle cell disease isn’t available currently, except for bone marrow transplantation, which needs a matching donor and involves serious risks and complications. Therefore, most people living with sickle cell disease depend on medications and blood transfusions to manage their symptoms and prevent further complications.
But now, gene therapy is providing a promising new way to treat sickle cell disease. Gene therapy for sickle cell disease targets the root cause of the disease by modifying the genes involved in hemoglobin production. There are various types of gene therapy techniques for sickle cell disease:
- Gene editing: This uses special tools like CRISPR-Cas9 to remove the flawed part of the hemoglobin gene and replace it with a normal sequence. This can restore the normal shape and function of hemoglobin and red blood cells.
- Gene addition: This involves adding a new gene that produces a protein that prevents or decreases the clumping of hemoglobin, improving the oxygen-carrying ability of red blood cells.
- Gene activation: This method involves turning on a gene that makes fetal hemoglobin, a type of hemoglobin produced only during the fetal stage. This fetal hemoglobin can counter the effects of sickle hemoglobin and protect red blood cells from turning into a sickle shape.
All these gene therapy approaches involve collecting stem cells that form blood from the patient’s bone marrow or blood, modifying them in a lab with viral or non-viral vectors (carriers that transport the genes), and then injecting them back into the patient. These modified stem cells then make healthy red blood cells that can lessen the symptoms and improve the condition of sickle cell disease.
Gene therapy for sickle cell disease is still in the early stages of research and testing, but it has shown encouraging results in various research studies.
Current Progress and Success Stories Gene Therapy for Sickle Cell Disease
Numerous clinical trials are going on to test the safety and effectiveness of gene therapy for sickle cell disease. Some of these trials have shown successful results, like reduced pain crises, improved blood counts and quality of life, and curing some patients of sickle cell disease. Here are some examples of these trials:
- A phase 1/2 trial performed by UCLA tested a gene addition method using a vector called LentiGlobin BB305 that carries an anti-sickling gene named βA-T87Q-globin. This trial reported stable production of anti-sickling hemoglobin in 11 out of 12 patients, who also experienced less pain crises, hospital stays, transfusions, and medication use. One patient was cured of sickle cell disease after receiving a bone marrow transplant from his brother, who had received the same gene therapy.
- A phase 1/2 trial conducted by NIH used a gene editing method with CRISPR-Cas9 to activate the fetal hemoglobin gene. The trial reported high levels of fetal hemoglobin in 9 out of 10 patients, who also experienced fewer pain crises, hospital stays, transfusions, and medication use. One patient had a serious adverse event, which was attributed to the chemotherapy and not the gene therapy.
- A phase 1/2 trial performed by Bluebird Bio used a gene addition method with a vector called LentiGlobin BB305 that carries a normal hemoglobin gene called βA-globin. The trial reported stable production of normal hemoglobin in 21 out of 22 patients, who also experienced fewer pain crises, hospital stays, transfusions, and medication use. One patient had a serious adverse event, which was attributed to the vector and not the gene therapy.
These trials show that gene therapy can be a possible and effective treatment for sickle cell disease, with some patients achieving long-term relief or cure. However, these trials also highlight some challenges and limitations of gene therapy, such as:
- The requirement of chemotherapy, which can cause side effects and complications like infections, infertility, and secondary cancers.
- The risk of toxicity related to the vector or unwanted changes in the DNA that can trigger cancers.
- The variability in the response and outcome of gene therapy, depending on the patient’s characteristics, the type and dose of vector, and the level and stability of hemoglobin expression.
- The cost and accessibility of gene therapy, which can be prohibitive for many patients and healthcare systems, particularly in low-resource settings where sickle cell disease is most common.
Therefore, more research and development are needed to improve the safety and effectiveness of gene therapy for sickle cell disease and to address the ethical, social, and economic issues associated with this novel treatment.
Challenges in Implementing Gene Therapy for SCD
Gene therapy is seen as a hopeful cure for sickle cell disease (SCD), a genetic issue that changes the shape and working of red blood cells. But, there are several difficulties in making this sickle cell anemia cure available and within reach for patients suffering from SCD.
Technical issues in gene therapy
A technical problem of gene therapy for sickle cell disease is getting the right gene to the cells it needs to target without causing any unwanted side effects. There are different ways of sending the gene, like viruses, nanoparticles, or electroporation. Each method has good and bad points, such as safety, efficiency, and accuracy. Another technical problem is making sure the changed cells can live and work properly in the patient’s body. This might require careful picking of the cells, fine-tuning of the gene editing tools, and keeping a close eye on the long-term results.
Ethical issues and debates about gene therapy
Gene therapy also raises ethical issues and debates, like who should get it, what it should cost, and what the potential risks and benefits might be. Some of the ethical concerns include:
- The chance of unexpected consequences or off-target effects of gene editing, like changing other genes or causing cancer.
- The consent and freedom of the patients, especially children or vulnerable groups, who may not completely understand or agree with the procedure.
- The fairness and equality of access to gene therapy for sickle cell, which could be limited by factors like availability, affordability, or eligibility rules.
- The social and cultural impacts of gene editing, like changing the identity or diversity of individuals or communities affected by SCD.
Financial obstacles and accessibility issues
Gene therapy is also expensive and complex, requiring specialized places and expertise. The expected cost of gene therapy for curing sickle cell anemia ranges from $500,000 to $1 million per patient. This creates a big financial obstacle for many patients with SCD, especially those living in low-resource settings or minority populations.
Also, gene therapy is not widely available or approved for SCD yet. Only a few clinical trials are currently underway or planned in different countries. So, there is a need to increase funding, research, and development of gene therapy for SCD and address regulatory, logistical, and ethical challenges that might limit its accessibility.
The Future of Sickle Cell Disease Treatment
Gene therapy has the ability to cure or greatly improve the life quality of patients with SCD. However, gene therapy alone might not be enough to address all the aspects of managing SCD. So, a complete approach that merges gene therapy with techniques for easing symptoms might be more helpful and beneficial for patients with SCD.
For instance, gene therapy might lower the need for frequent blood transfusions and the risk of iron overload or alloimmunization. Gene therapy might also increase the response to hydroxyurea and the production of fetal hemoglobin. Gene therapy might also improve the immune system and the ability to fight infections.
Current Research
The cure for sickle cell disease (SCD) could be around the corner thanks to gene therapy. This innovative method focuses on fixing or tweaking the error in the gene responsible for the abnormal shape and function of red blood cells (RBCs).
Notable achievements in the cure for sickle cell anemia through gene therapy include:
- The first patient treated with CRISPR-Cas9 gene editing in 2019. The patient showed a stable improvement in hemoglobin levels and reduced pain incidents two years later.
- A gene therapy product named LentiGlobin. It introduces an anti-sickling gene to the patient’s own stem cells and has proven to be effective and safe in numerous clinical trials.
- A gene therapy strategy that activates fetal hemoglobin by silencing a suppressor gene named BCL11A. It has shown promising results in decreasing vaso-occlusive crises and transfusion needs in patients with SCD.
The cure for sickle cell could overcome some drawbacks and dangers of the current standard care methods. Gene therapy could offer a more tailored, long-lasting solution for SCD patients who don’t have a suitable donor or can’t handle the transplant procedure and its side effects.
FAQs
Is Sickle Cell Disease Inherited or Acquired?
Sickle cell disease is inherited, not acquired. It occurs when a child inherits two mutated HBB genes, one from each parent, leading to the production of abnormal hemoglobin that causes the red blood cells to become sickle-shaped.
At What Age Does Sickle Cell Get Worse?
Sickle cell disease symptoms can appear as early as 4 months old, but its severity can vary. Complications tend to increase and become more severe in adulthood, as the cumulative effects of the disease take their toll on the body.
Can White People Get Sickle Cell Anemia?
Yes, white people can get sickle cell anemia, although it is more prevalent in people of African, Middle Eastern, Indian, and Mediterranean descent. Sickle cell anemia is a genetic disease that depends on inheriting specific gene mutations, regardless of ethnicity.
Can a Child Have Sickle Cell Trait if Neither Parent Has It?
A child cannot have the sickle cell trait if neither parent has it. The trait occurs typically when the child inherits one sickle cell gene. If neither parent has the trait or disease, they cannot pass the gene to their children. Theoretically, a child may get sporadic or de-novo mutations, but such cases are practically non-reported.
What is the Life Expectancy of a Sickle Cell Patient?
Advancements in treatment have improved life expectancy for sickle cell patients, with many living into their 50s and beyond. Early diagnosis and comprehensive care are crucial for managing complications and improving quality of life.
What are the 1st Signs of Sickle Cell Crisis?
The first signs of a sickle cell crisis often include severe pain, which can occur in the chest, abdomen, limbs, or joints. Other early symptoms may include fatigue, fever, and swelling in the hands or feet, indicating a vaso-occlusive crisis.
Final Words
Sickle cell disease is a genetic disorder that causes intense pain, damage to organs, infections, and early death due to red blood cells’ abnormal shape and function.
Gene therapy is a new and exciting approach that offers hope in curing or treating SCD by fixing or altering the faulty gene causing the sickle shape in RBCs. Gene therapy could provide a better alternative to the current treatment methods.
Despite the significant progress and success of gene therapy for sickle cell anemia cure, there are still challenges that must be resolved before it can become widely available and affordable for patients who need it.
References:
- https://www.mayoclinic.org/diseases-conditions/sickle-cell-anemia/symptoms-causes/syc-20355876
- https://www.cdc.gov/ncbddd/sicklecell/facts.html
- https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/what-gene-therapy
- https://www.healthline.com/health/sickle-cell-anemia-gene-therapy
- https://www.cuimc.columbia.edu/news/experimental-gene-therapy-reverses-sickle-cell-disease-years
- https://www.mayoclinic.org/tests-procedures/gene-therapy/about/pac-20384619
- https://ashpublications.org/hematology/article/2021/1/174/482932/Gene-therapy-for-sickle-cell-disease-where-we-are
- https://pubmed.ncbi.nlm.nih.gov/34232993
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6123269

Dr. Sumeet is a seasoned geneticist turned wellness educator and successful financial blogger. GenesWellness.com, leverages his rich academic background and passion for sharing knowledge online to demystify the role of genetics in wellness. His work is globally published and he is quoted on top health platforms like Medical News Today, Healthline, MDLinx, Verywell Mind, NCOA, and more. Using his unique mix of genetics expertise and digital fluency, Dr. Sumeet inspires readers toward healthier, more informed lifestyles.