Thalassemia is an inherited blood disorder. It interferes with the production of hemoglobin, a protein in red blood cells that carries oxygen.
Thalassemia affects millions of people worldwide, especially in regions where malaria is common, such as Asia, Africa, and the Mediterranean. According to the World Health Organization (WHO), about 5% of the world’s population carries a gene for thalassemia, and about 300,000 children are born with severe forms of thalassemia each year.
In this article, we will describe thalassemia’s genetics, symptoms, and how it works, as well as discuss the advantages and challenges of prenatal genetic testing and disease management.
Quick Overview:
This disorder is due to mutations in the genes that create two types of chains for hemoglobin: alpha and beta.
These mutations result in not enough or abnormal hemoglobin, leading to thalassemia anemia, a condition where the blood doesn’t have enough oxygen for the body’s needs.
To tackle thalassemia, prenatal genetic testing, and disease management are important. Prenatal genetic testing helps identify couples who risk having a child with thalassemia, providing options such as preimplantation genetic diagnosis (PGD), prenatal diagnosis (PND), or genetic counseling.
Read on to know all about this disorder including how it is managed.
Understanding Thalassemia
Thalassemia Genetics
Thalassemia is caused by mutations in the DNA of cells that produce hemoglobin. The two main types of thalassemia are alpha thalassemia and beta thalassemia. Each type impacts a different chain of hemoglobin.
Alpha Thalassemia
Alpha thalassemia happens when one or more of the four genes that create the alpha chain of hemoglobin are deleted or mutated. The severity of alpha thalassemia depends on how many genes are impacted.
- If one gene is affected, there are no symptoms. This condition is known as a silent carrier or alpha-thalassemia minima.
- If two genes are affected, there may be minor thalassemia or mild anemia. This is called alpha-thalassemia trait or alpha-thalassemia minor.
- If three genes are affected, there is moderate to severe anemia. This condition is known as hemoglobin H disease or alpha-thalassemia intermedia.
- If all four genes are affected, there is no production of alpha chains. This condition is known as hydrops fetalis or alpha-thalassemia major, which is usually fatal before or shortly after birth.
Beta Thalassemia
Beta thalassemia happens when one or both of the two genes that create the beta chain of hemoglobin are mutated. The mutations can reduce or prevent the production of beta chains. The severity of beta thalassemia depends on the type and location of the mutation.
- If one gene is affected, there may be minor thalassemia or mild anemia. This condition is known as beta-thalassemia minor or beta-thalassemia trait.
- If both genes are affected, there is severe anemia. This condition is known as beta-thalassemia major or Cooley’s anemia.
Symptoms of Thalassemia
The symptoms of thalassemia depend on the type and severity of the disorder. The main symptom of thalassemia is anemia, which can cause tiredness, weakness, pale or yellowish skin, shortness of breath, dark urine, and abdominal swelling. Anemia can also affect the growth and development of children with thalassemia.
Other symptoms and complications of thalassemia include:
- Bone deformities, especially in the face and skull, due to increased bone marrow activity and expansion.
- An enlarged spleen, due to the immune system removing abnormal red blood cells.
- Heart problems, such as irregular heart rhythms, cardiomyopathy, and heart failure, due to chronic anemia and iron overload.
- Liver problems, such as cirrhosis, hepatitis, and liver cancer, due to iron overload and viral infections.
- Infections, due to impaired immunity and exposure to blood-borne pathogens.
- Osteoporosis, due to reduced bone density and calcium absorption.
- Endocrine problems, such as diabetes, underactive thyroid, underactive parathyroid, and underactive sex glands, due to iron overload and hormonal imbalances.
- Thrombosis, due to abnormal blood clotting and inflammation.
Pathophysiology of Thalassemia
Thalassemia disrupts the normal creation and function of hemoglobin. Hemoglobin is a complex protein made of four globin chains (two alpha and two beta) and four heme groups (iron-containing molecules that bind oxygen).
The globin chains are encoded by genes on chromosomes 16 (alpha) and 11 (beta). Hemoglobin creation requires a balanced production of alpha and beta chains. When one type of chain is deficient or abnormal, the other type accumulates and forms unstable or ineffective hemoglobin molecules.
alpha thalassemia
In alpha thalassemia, the lack of alpha chains leads to the creation of excess beta chains, which form groups called hemoglobin H. This form of hemoglobin is unstable and likely to be oxidized, which damages the red blood cells and shortens their lifespan.
In severe cases of alpha thalassemia, such as hydrops fetalis, there is no production of alpha chains at all. This causes the creation of gamma chains (normally present in fetal hemoglobin), which form groups called hemoglobin Barts. This form of hemoglobin has an extremely high affinity for oxygen, which prevents oxygen release to the tissues. This causes severe hypoxia and tissue damage in the fetus.
beta thalassemia
In beta thalassemia, the lack or defect of beta chains leads to the creation of excess alpha chains, which accumulate in the red blood cells and cause damage. This also inhibits the production of normal hemoglobin molecules. The reduced or absent production of normal hemoglobin causes anemia and hypoxia in the tissues.
The chronic anemia caused by thalassemia prompts the bone marrow to produce more red blood cells. However, the bone marrow cannot meet the demand for red blood cells, leading to the production of immature or abnormal red blood cells. This results in more anemia and iron deficiency.
Treatment for thalassemia often involves regular blood transfusions to correct anemia and improve oxygen delivery to the tissues. However, blood transfusions can also introduce excess iron into the body, which can accumulate in various organs and cause damage. To prevent iron overload, people with thalassemia must take medications that bind and regularly remove iron from the body.
Prenatal Genetic Testing for Thalassemia
Thalassemia anemia can be mild or serious, depending on what type and how many changes or mutations there are in the genes that cause it.
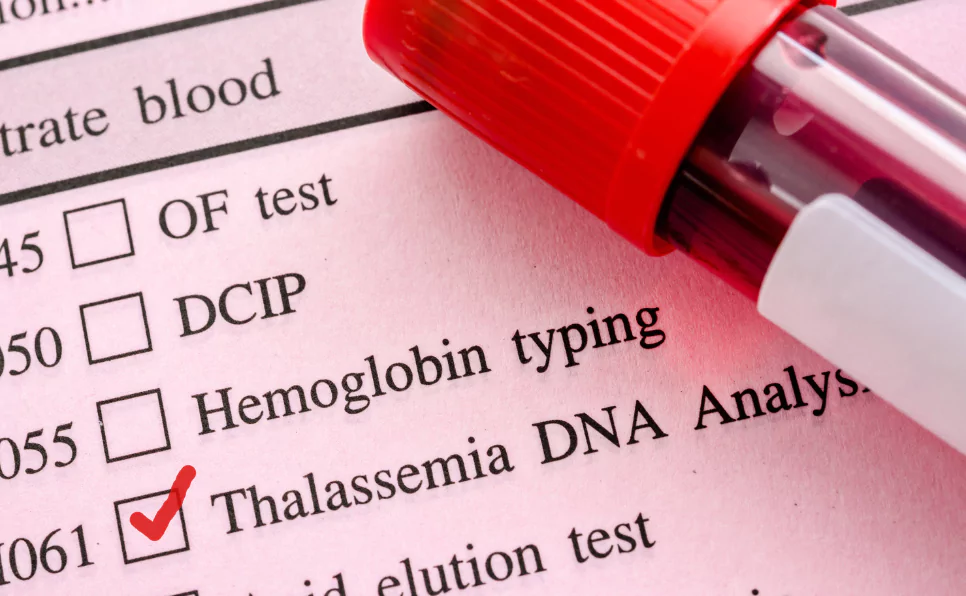
Importance of Prenatal Genetic Testing
Testing for thalassemia in a baby before they’re born, also known as prenatal genetic testing, can help parents prepare for the baby’s medical needs and make well-informed decisions about the pregnancy.
This thalassemia testing can also stop the condition from being passed down to future generations by finding out if parents are carriers of the thalassemia trait and providing them with choices for having children.
For carrier couples planning a family, preimplantation genetic diagnosis (PGD) combined with in vitro fertilization (IVF) can ensure only embryos free from thalassemia are implanted. These interventions, however, are technically complex and can be emotionally and financially demanding.
Methods of Prenatal Genetic Testing
There are several ways to test for thalassemia before a baby is born, depending on how far along the pregnancy is and what resources are available. The most usual methods are:
- Amniocentesis
This is a procedure where a small amount of fluid that surrounds the baby, called amniotic fluid, is taken with a thin needle that’s inserted through the belly. This fluid has cells from the baby that can be checked for thalassemia genetics. This test is typically done between 15 and 20 weeks of pregnancy.
- Chorionic Villus Sampling (CVS)
This is a procedure where a small sample of tissue from the placenta, which is the organ that connects the baby to the mother’s blood supply, is taken using a thin tube inserted through the cervix or a needle inserted through the belly. The tissue has cells from the baby that can be checked for thalassemia genetics. This test can be done earlier than amniocentesis, between 9 and 12 weeks of pregnancy.
- Non-invasive Prenatal Testing (NIPT)
This is a blood test that looks at fragments of the baby’s DNA that are present in the mother’s blood. This test can identify some types of thalassemia genes very accurately, but it can’t find all possible mutations or tell how severe the disease is. This test can be done as early as 10 weeks of pregnancy.
Interpreting Prenatal Genetic Testing Results
The results of thalassemia prenatal diagnosis depend on whether the baby has inherited one or two copies of the disease-causing gene mutations from each parent. The possible outcomes are:
- Normal: The baby has no thalassemia genes and will not have the disease or be a carrier.
- Carrier: The baby has one copy of a thalassemia gene and will not have symptoms but can pass it on to his or her children, which is known as having a minor thalassemia or thalassemia trait.
- Affected: The baby has two copies of a thalassemia gene and will have symptoms that can vary in severity depending on the type of mutation.
To make sure the results of prenatal thalassemia screening are accurate, they are always confirmed to eliminate any errors or contamination.
Ethical and Social Considerations in Prenatal Genetic Testing
Doing prenatal genetic testing for thalassemia brings up some ethical and social issues that parents should think about before doing the test. Some of these issues are:
- The mental impact of knowing that the baby has thalassemia or is a carrier, and how it might affect the relationship between the parent and the child.
- The availability and accessibility of treatment and care for thalassemia, especially in places with fewer resources.
- The potential for discrimination or negative attitudes towards people with thalassemia or carriers in some cultures or communities.
- The personal and religious beliefs about abortion, adoption, or other options for having children if the baby has thalassemia.
Deciding to do prenatal genetic testing for thalassemia is a personal decision that should be made after talking to a genetic counselor, a doctor, and other trusted sources of information and support.
Disease Management for Thalassemia
In thalassemia, the body struggles to produce enough hemoglobin, leading to anemia, which can leave the patient feeling tired, pale, and weak overall. This condition has two central types: alpha thalassemia and beta thalassemia.
Early Management Strategies
When it comes to early management strategies for thalassemia, the primary focus is to prevent or manage anemia and an excess of iron (iron overload) in the body, which are common troubles linked to this condition. There are two main treatments:
- Iron chelation therapy: This is medicine that aids in removing surplus iron from the body. Too much iron can harm crucial organs like your heart and liver. Iron chelation therapy can be taken by mouth, injection, or infusion, and the type and dosage depends on how severe the iron overload is and what the patient prefers.
- Blood transfusions: This procedure involves replacing the patient’s blood with donor blood. Blood transfusions can boost the level of hemoglobin, alleviating the symptoms of anemia. But, they also increase the chance of iron overload, which is why they need to be used alongside iron chelation therapy. The frequency and volume of blood transfusions depend on the type and seriousness of the thalassemia.
Handling Thalassemia in the Long Run
The main goal of long-term management strategies for thalassemia is to either cure the condition or reduce its complications. There are two main treatments:
- Bone marrow transplantation: This is a procedure where the patient’s bone marrow is replaced with healthy bone marrow from a donor. Bone marrow is the soft tissue inside our bones that makes blood cells. Bone marrow transplantation can cure thalassemia by restoring normal hemoglobin production. However, it’s a risky treatment and requires a compatible donor, which isn’t always available. The patient also needs to take medicines to suppress their immune system to prevent rejection of the donor bone marrow.
- Gene therapy: This experimental treatment aims to fix the genetic defect causing thalassemia. Gene therapy involves inserting a normal copy of the affected gene into the patient’s bone marrow cells using a virus or other vector. The modified cells are then returned to the patient’s body, where they can produce normal hemoglobin. Gene therapy for Thalassemia has shown promise in some trials, but it’s still being developed and isn’t widely available.
Supportive Therapies to Improve Quality of Life
Apart from the main treatments, some supportive therapies can help improve the quality of life and prevent complications for people with thalassemia. These include:
- Folic acid supplements: Folic acid is a vitamin that helps make new red blood cells. People with thalassemia may need extra folic acid to prevent or treat folate deficiency anemia, which can worsen their condition.
- Vaccinations: People with thalassemia are more susceptible to infections due to their weakened immune system and spleen function. Vaccinations can protect them from common diseases such as the flu, pneumococcal pneumonia, hepatitis B, and meningococcal meningitis.
- Surgery: Some individuals with thalassemia may need surgery to remove their spleen or gallbladder if these organs become too big or start causing problems. Surgery can relieve pain and prevent complications such as bleeding or infection. However, surgery also carries risks and may require lifelong antibiotics or blood thinners after removal of the spleen or gallbladder.
Lifestyle Changes
There are certain lifestyle changes that can help people with thalassemia cope better with their condition and improve their well-being:
- Maintaining a balanced diet: A nutritious diet provides the necessary nutrients and energy for growth and development. People with thalassemia should avoid iron-rich foods or supplements, as they can worsen iron overload.
- Regular exercise: Physical activity can improve blood circulation, muscle strength, bone health, and mood. People with thalassemia should avoid strenuous or high-impact exercises that can cause injury or bleeding.
- Managing stress and emotions: Living with thalassemia can be stressful and challenging, especially for children and adolescents. Seeking emotional support from family, friends, counselors, or support groups can be very beneficial.
While thalassemia is a lifelong condition that requires regular monitoring and treatment, with the right care and management, individuals with thalassemia can lead fulfilling and productive lives.
The Psychological Impact of Thalassemia and Ways to Deal With It
Individuals with thalassemia major, the most severe form of thalassemia, need regular blood transfusions to avoid serious anemia and harm to their organs.
However, these transfusions can result in an overload of iron, leading to significant health complications. Living with thalassemia can have a strong emotional impact on both patients and their families, influencing their emotional health, quality of life, and ability to interact socially.
Emotional Effects on Patients
Individuals with thalassemia major face numerous challenges and hurdles throughout their lives, such as frequent hospital visits, painful treatments, physical restrictions, stigma, discrimination, and uncertainty about their future.
These stress factors can lead to a variety of emotional issues, such as depression, anxiety, anger, low self-esteem, and poor coping abilities. Research has shown that those with thalassemia major have lower life satisfaction and happiness levels than healthy individuals. They may also experience feelings of guilt, shame, isolation, and hopelessness.
Impact on Family Members
Thalassemia doesn’t just affect the patients, but also their family members who provide care and support. Family members might feel emotional stress, financial strain, fatigue from caregiving, marital issues, and diminished social activities due to the requirements of caring for someone with a long-term illness like thalassemia.
They might also have to grapple with the fear of losing their loved one or the possibility of having another child with thalassemia. Additionally, family members might have to address their own feelings of guilt, anger, resentment, or grief related to the genetic nature of thalassemia.
Psychological Support and Counseling
Given the complex and multi-layered emotional impact of thalassemia on patients and their families, it is crucial to provide them with adequate psychological support and counseling services.
Psychological interventions can help patients and family members manage their emotions, boost their self-esteem and resilience, enhance their communication and problem-solving abilities, and increase their commitment to treatment.
Psychological support can be provided in various forms and settings, such as one-on-one or group therapy, family therapy, cognitive-behavioral therapy, relaxation techniques, art therapy, or online platforms.
Patient Support Groups and Communities
Another important source of emotional support for people with thalassemia and their families is patient support groups and communities. These groups offer a safe and supportive environment where patients and family members can share their experiences, emotions, concerns, and information with others who understand their situation.
They can also offer practical advice, emotional encouragement, social networking, advocacy, and education on various aspects of thalassemia. Healthcare professionals, non-profit organizations, or patient associations at local or national levels can organize patient support groups and communities.
Progress in Thalassemia Research and Treatment
Despite the challenges and complications linked with thalassemia major, there is hope for patients and their families as research and treatment options continue to evolve.
In recent years, there have been substantial advances in gene therapy for thalassemia major, which aims to correct the defective gene that leads to the disease.
Gene therapy has the potential to provide a permanent cure for thalassemia major, eliminating or reducing the need for blood transfusions and improving patients’ quality of life.
Recent Developments in Gene Therapy
Gene therapy for thalassemia major involves taking stem cells from the patient’s blood and inserting a functional gene into their DNA using a viral vector. After removing the abnormal genes, the modified stem cells are reintroduced into the patient’s body. The functional gene enables the stem cells to generate normal hemoglobin and restore healthy blood production.
Several clinical trials have been conducted to test the safety and efficacy of gene therapy for thalassemia major. One of them is Beti-cel (brand name Zynteglo), which was approved by the European Medicines Agency in 2019 for patients aged 12 years or older who require regular transfusions.
A recent phase-3 clinical trial showed that Beti-cel was able to stop or significantly reduce the transfusion dependence of 20 out of 22 treated patients, including 6 out of 7 children under 12 years old. Another gene therapy that is being developed is LentiGlobin, which has shown promising results in early-stage trials.
Potential Future Treatments
Gene therapy for thalassemia major is still a novel and costly treatment that isn’t widely available or accessible to all patients. There are also some challenges and risks associated with gene therapy, such as the possibility of viral infection, immune reaction, or cancer development.
Therefore, researchers are working on improving gene therapy’s safety, efficacy, and affordability for thalassemia major and exploring other potential treatments.
Some of the future directions for thalassemia research and treatment include:
- Developing new viral vectors or gene editing tools that can deliver the functional gene more precisely and efficiently.
- Using stem cells from other sources, such as umbilical cord blood or induced pluripotent stem cells, to overcome the limitations of autologous stem cells.
- Combining gene therapy with other therapies, such as immunosuppression or iron chelation, to enhance the outcomes and reduce the complications.
- Finding alternative ways to increase fetal hemoglobin production, which can compensate for the lack of adult hemoglobin in thalassemia patients.
Final Words
Thalassemia is a severe genetic disorder, and patients require lifelong blood transfusions and iron chelation therapy to survive, but these treatments also have side effects and limitations. Thalassemia major also deeply affects patients and their families emotional well-being, quality of life, and social interactions.
Prenatal genetic testing is an important tool to prevent the transmission of thalassemia major to future generations. It can help couples at risk of having a child with thalassemia major make informed decisions about their reproductive options. Prenatal genetic testing can also help diagnose thalassemia major in early pregnancy and prepare for proper management and treatment.
By supporting research on thalassemia major, we can help progress the scientific knowledge and innovation that can lead to better outcomes and quality of life for patients.
References:
- https://www.cdc.gov/ncbddd/thalassemia/facts.html
- https://www.nhlbi.nih.gov/health/thalassemia
- https://www.mayoclinic.org/diseases-conditions/thalassemia/symptoms-causes/syc-20354995?p=1
- https://www.sciencedirect.com/science/article/abs/pii/S1521693416301195
- https://www.mayoclinic.org/diseases-conditions/thalassemia/diagnosis-treatment/drc-20355001
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8837879/
- https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-021-00547-0
- https://www.researchgate.net/publication/271705038_Affective_Control_and_Life_Satisfaction_in_Thalassemics
- https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-019-1466-y
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3425167/
- https://www.nejm.org/doi/full/10.1056/NEJMe2118580
- https://www.nature.com/articles/d43978-022-00010-7
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6765258/
- https://www.labiotech.eu/trends-news/thalassemia-gene-therapy-approval/
- https://www.frontiersin.org/research-topics/49210/psychological-issues-in-patients-with-thalassemia-and-sickle-cell-disease-and-their-families-and-caregivers
- https://www.chop.edu/news/fda-approves-first-potentially-curative-gene-therapy-beta-thalassemia

Dr. Sumeet is a seasoned geneticist turned wellness educator and successful financial blogger. GenesWellness.com, leverages his rich academic background and passion for sharing knowledge online to demystify the role of genetics in wellness. His work is globally published and he is quoted on top health platforms like Medical News Today, Healthline, MDLinx, Verywell Mind, NCOA, and more. Using his unique mix of genetics expertise and digital fluency, Dr. Sumeet inspires readers toward healthier, more informed lifestyles.